Social determinants of health (SDOH) are nonmedical factors that influence a wide range of health outcomes and risks. These include economic stability, housing conditions, education, healthcare access, quality of the built environment, and community context.
Additionally, the nature of occupations that Georgia Latinos are most likely to have—construction, hospitality, entrepreneurship—are less likely to offer employee benefits like health insurance and paid sick leave. And they may not pay well enough to purchase other insurance options.
The 2023 Health Status of Latinos in Georgia Report, published by the Latino Community Fund (LCF Georgia), offers a detailed snapshot of our community's health outcomes across multiple dimensions of well-being.

Immigration Status as a Social Determinant of Health
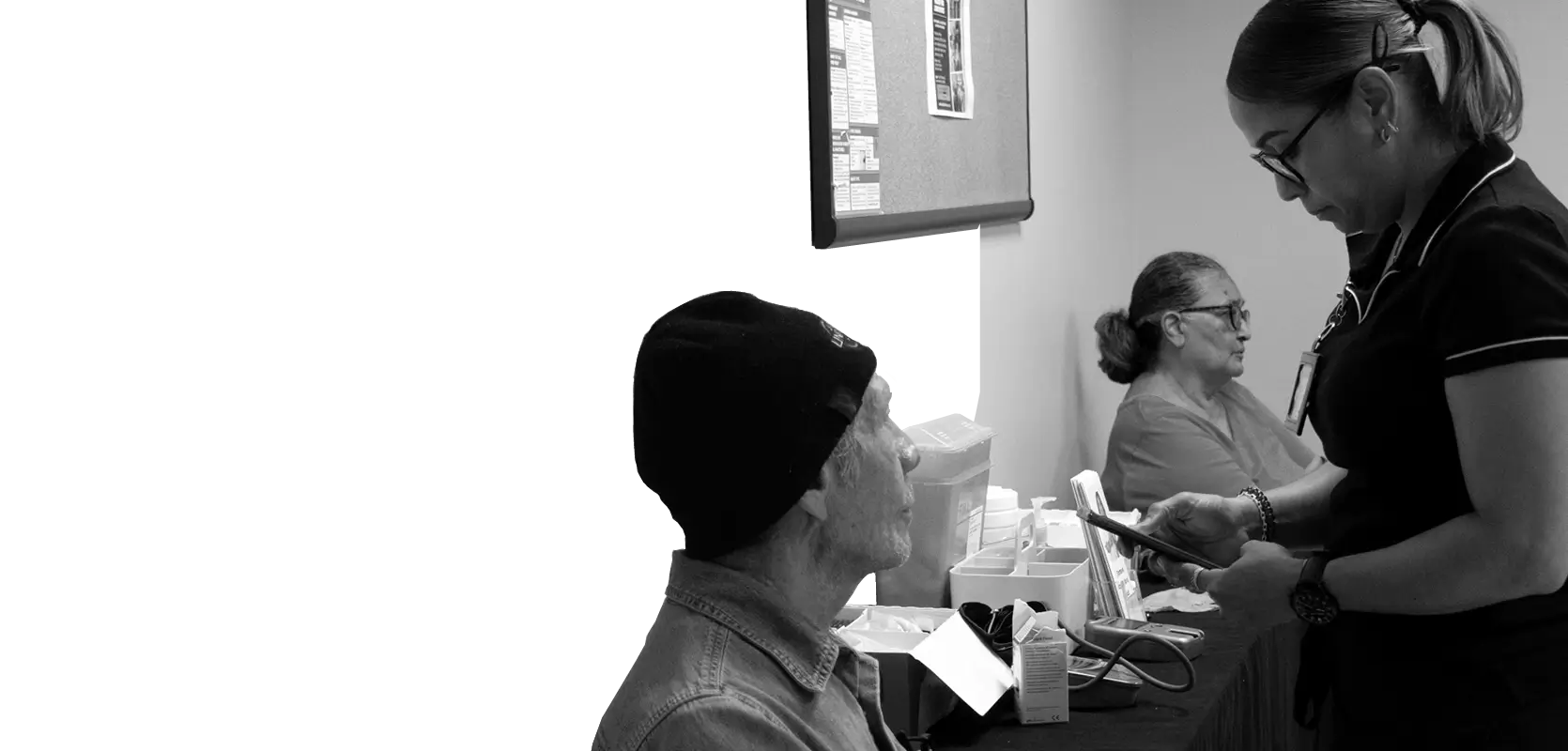
While low-cost clinics may be available, accessing their services can be difficult. Many of us, particularly gig workers and independent contractors, struggle to provide the necessary proof of employment or income to qualify for care.

We were two—my brother and I—and that helped us take care of my mom. One alone couldn't do it. I had to almost stop working to support my mother during her sickness.
Mauri Maza
Mauri lives in Lawrenceville. She moved from Venezuela to Georgia ten years ago, followed by her mother about four years later. Soon after she moved in, Mauri’s mother was diagnosed with cancer. For years, they faced the challenges of navigating the U.S. healthcare system as an immigrant family.
Anti-immigrant legislation significantly impacts healthcare access for Latinos, leading to both direct and indirect effects. Many individuals miss medical appointments or delay seeking care because they cannot drive without a license. Additionally, Latinos often fear filling out Medicaid application forms that require information about their family's immigration status.
We were always scared of messing something up because of the language barrier.
Mauri Maza
In some cases, families find financial support through hospitals, as was the case for Mauri’s mother, who didn't have insurance. However, maintaining this support requires renewing documentation every six months, demanding considerable time and effort for paperwork.
Current laws that prevent obtaining driver’s licenses make it harder for some immigrants to access healthcare. Many individuals miss hard-to-schedule appointments because they cannot drive themselves, lack a driver, or cannot afford taxi fares.
A beneficial change for Latinos would be a Medicaid expansion that provides coverage for all residents, regardless of immigration status.
A Closer Look at Vulnerable Groups
Where we work and what we do are key to understanding our health risks, especially for those in high-risk jobs like agriculture, poultry processing, construction, manufacturing, hospitality, cleaning, and service work. Many of these workers feel they "can’t afford to be sick," which forces them to show up even when they're not feeling well just so they can make a living.
I had a really bad time with COVID. I didn't want to go to the doctor because I didn't have insurance, but I was feeling really bad. I was hospitalized and could barely move. My only goal was to recover so I could go to work and bounce back.
Henry Reyes
During the height of the COVID-19 pandemic, Latino individuals experienced significant health disparities driven by social determinants of health, and were nearly three times more likely to be hospitalized compared to non-Hispanic white individuals35. Popular Latino occupations, like construction, hospitality, and healthcare, required continued in-person presence throughout the pandemic.
Despite being considered essential workers, farm workers had limited access to COVID testing and support during the pandemic36.
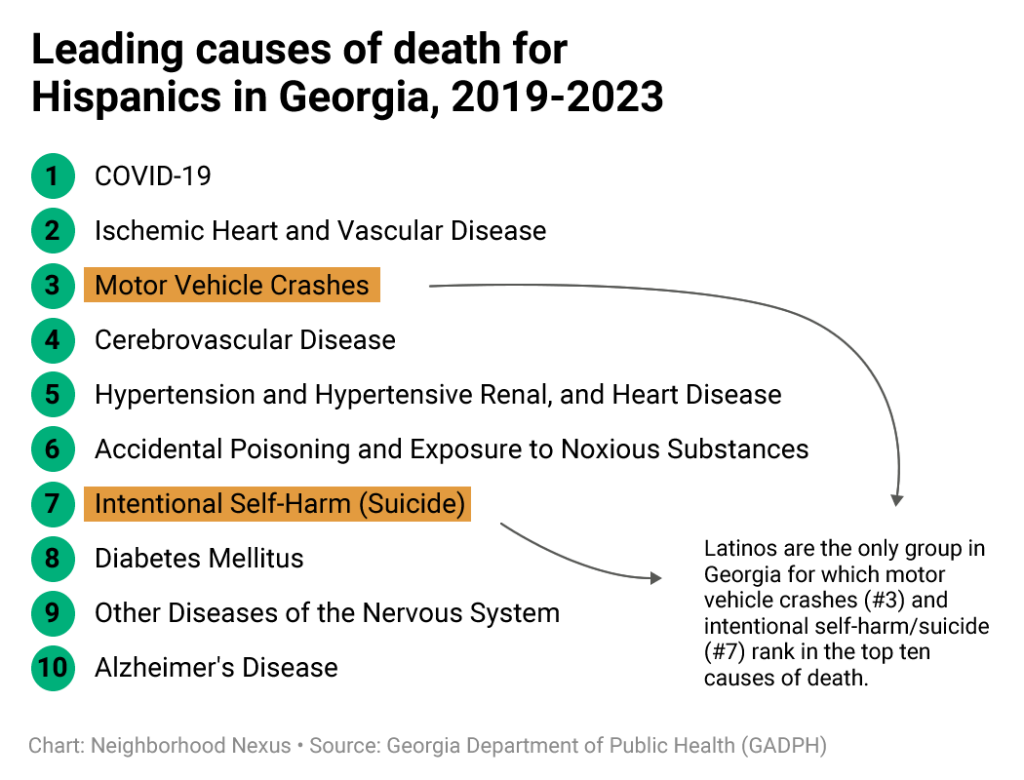
From 2018 to 2022, COVID-19 was the leading cause of death for Latinos in Georgia.
These high-risk jobs often come with serious hazards, like exposure to chemicals, dangerous machinery, and unsafe conditions. Roxana Chicas, professor at Emory University, explains that farmworkers are 35 times more likely to die from heatstroke, leading to a shorter life expectancy compared to the general workforce. It is important to note here that Georgia is a major state for H-2A workers, most of whom are Latino37.
Pregnant women represent a particularly vulnerable population, facing significant risks from adverse social determinants of health that can impact both their well-being and that of their babies. Connecting Latina women and other women of color to medical and mental health services is crucial for ensuring maternal and infant health.

In one of the most dangerous states to be pregnant38, Latina women carry even more risk. In 2022, 11.4% of live births to Hispanic mothers in Georgia received late or no prenatal care, compared to 7.6% for non-Hispanic mothers. Additionally, 22.4% of births to Hispanic mothers had an inadequate Kotelchuck index, compared to 15.9% for non-Hispanics39.
The Kotelchuck measure is an index of the adequacy of prenatal care based on the month of entry, the number of prenatal visits, and the infant's gestational age at birth.
When receiving prenatal care, one significant medical challenge for Latina women is gestational diabetes. While this condition can often be managed through dietary changes, many recommendations do not take cultural differences into consideration. Roxana Chicas shares that Latina women often feel judged by healthcare providers who lack cultural awareness. In contrast, Latino doctors tend to have more open and supportive conversations about diet modifications.
Alternatives for the Community
In Latin America, healthcare carries significant emotional and spiritual value, especially when caring for family members like children or the elderly. For this reason, health and faith are deeply intertwined in our community. This contrasts sharply with the U.S. healthcare system, which prioritizes efficiency over relational connections. This difference helps explain the distrust some patients feel towards providers who approach healthcare with a transactional mindset, while patients often seek deeper, more holistic support.
In their search for mental health support or physical therapy, individuals may end up consulting life coaches, chiropractors, or spiritual counselors. While these practitioners can offer value, they may not be qualified to address serious underlying health issues.
Due to high healthcare costs in the U.S., many Latinos bring medications from their home countries—such as antibiotics and birth control—when they visit.
This practice can be convenient and cost-effective for treating common ailments but carries significant risks, especially with antibiotics.
Despite these preferences, healthcare professionals, particularly doctors, remain trusted figures and natural leaders within these communities. Their recommendations hold considerable weight and can significantly influence health-seeking behaviors.
Accessing healthcare information in their preferred language is a major challenge for many in the Latino community, often leading to confusion or even scams. Even though federal laws require language support, it’s not always implemented effectively, leaving many people without the help they need.
A common issue is that children are asked to translate for their parents during medical visits. This can create big communication problems and raise ethical concerns. It puts a heavy emotional load on kids, which can lead to stress and trauma, especially if sensitive topics come up. It can also affect the relationship between parents and their children.
I grew up translating for my parents, not only in school but also in doctor's appointments or reading bills
Leslie Gutierrez
Breaking Barriers in Mental Health
It was hard for my mom to get an insurance because of her migratory status. Navigating both the health system and immigration process at the same time was very taxing for us.
Mauri Maza

Latinos in the U.S., especially in Georgia, face unique mental health challenges due to a mix of cultural, economic, and systemic issues. Barriers like stigma, lack of insurance, and language difficulties make these problems even tougher.
However, there's been some progress, as more community members open up to treatment and diagnosis since the COVID-19 pandemic began.
Culturally, Latinos may be less receptive to medication than other groups, even when it's necessary. Yet, when healthcare providers take the time to communicate openly and respectfully with families, trust can grow, easing concerns about medication.
Latino parents are generally eager for mental health services for their kids, often prompted by teachers at school or law enforcement. However, even when Latino students report mental health challenges such as depression or anxiety, many find it difficult to attend counseling sessions due to work commitments.
How schools address behavioral issues varies widely, largely based on their access to resources and capacity. Some schools provide support resources, while many others lean toward strict discipline. Unfortunately, even minor infractions can lead to suspensions and arrests, creating traumatic experiences while squashing future opportunities.
To effectively support these students, providers need to reach them where they are, bringing testing sites and mobile clinics into the community. Parent support and guidance groups have also proven to help Latino families navigate the mental health support system more effectively.
Georgia ranks 47 out of 50 in access to mental health services40. For Latinos—especially immigrant families and those who speak only Spanish—access is even more limited, with very few fully licensed Spanish-speaking mental health providers available41.
While children can usually get the help they need—thanks to their U.S. citizenship or government coverage—parents frequently find it hard to access the same services for themselves, mainly because of a lack of health insurance.
Latino kids who identify as LGBTQ+ face extra challenges, often struggling to engage with parents who may not fully understand their experiences, particularly regarding mental healthcare.
Ser Familia has been collecting Adverse Childhood Experiences (ACEs) questionnaires for more than eight years. Their data shows a significant prevalence of ACEs among the Latino community they serve. These findings emphasize the widespread impact of ACEs within the Latino population in Georgia and the need for targeted interventions to address their long-term effects on mental health.
Adverse Childhood Experiences (ACEs) are traumatic events that occur before a child turns 18. These experiences include various forms of abuse, neglect, and household dysfunction, such as parental substance use, incarceration, and domestic violence. Experiencing ACEs has been linked to a range of negative outcomes in adulthood, including poor physical and mental health. Nationally, about 64% of adults report experiencing at least one ACE during childhood.
A System of Support
Latinos tend to rely on one another when seeking mental health services or facing challenges in accessing healthcare, especially from someone in our community who can drive us and speak both English and Spanish.
Just like finding job opportunities and housing, we often discover vital information about financial help, health guidance, and healthy living within the community. For example, many Latino-serving businesses act as local hubs, distributing information about organizations like Ser Familia, which provide assistance to Latino families in navigating health concerns and finding providers that fit their needs.
Mutual support and strong community networks play a vital role in the well-being of Latinos, whether navigating mental health challenges or accessing physical health services. Though frequently unseen, these informal networks serve as an invaluable asset within our community. By leaning on each other—through family ties and community relationships—we create a support system that helps us overcome challenges and improve our overall health.